What is HPV?
The Human Papilloma Virus (HPV) is not one virus, but a family of about 200 different ones that cause common warts, genital warts and some cancers.
The majority of sexually active adults acquire at least one variety of HPV and it’s a near universal infection in people with HIV. Even people with one lifetime partner can get HPV, if their partner has it.
Most people clear the virus from their bodies within a one to two-year period.
About 40 types of HPV are passed on through sexual contact. It is important to realise though, that the virus can be spread through skin-to-skin contact that doesn’t involve penetrative sex. Condoms will not necessarily fully protect people from coming into contact with it.
Back to top
HPV-related diseases
For most people, HPV will cause them no harm. Only specific varieties of HPV cause cancer and even if you do come in contact with these, the chances of developing cancer are very small.
Some people do not clear the virus from their bodies, and this can cause:
- Genital warts on the penis, anus or vagina. It is also possible to have these types of warts on the lips and in the mouth.
- Cancer of the anus, cervix, penis vagina, vulva and oropharynx (back of the throat, including the base of the tongue and tonsils).
ANAL CANCER IS ONE OF THE MOST COMMON CANCERS FOR PEOPLE LIVING WITH hiv.
Although some other strains of HPV are associated with cancers, two main strains of HPV – HPV 16 and HPV 18 – cause 70% of cervical cancers and over 80% of anal cancers worldwide.
It is estimated that HPV is responsible for about 5% of cancers worldwide. However, anal cancer is one of the most common cancers for people living with HIV.
Back to top
HPV and Gay Men
This resource has been developed for gay men because they are at a significantly higher risk than the general population of developing anal cancer.
Every year anal cancer is diagnosed in about two people per 100 000 in the general population.
Men who have sex with men are about 20 times more likely than heterosexual men to develop anal cancer, and HIV-positive men who have sex with men are even more likely (up to 100 times more than the general community).
Back to top
Can HPV be prevented?
Condoms can lower your chances of picking up HPV. However, as HPV can infect areas of the body not covered by condoms, they are not fully protective against the virus. Fingers and sex toys involved with anal sex play, as well as oral sex, may pass on HPV, too.
Vaccines have been developed to protect against HPV, including the strains which are most likely to cause anal cancer. They are most effective if given before people become sexually active.
New vaccines are currently being developed to protect against even broader ranges of strains of HPV.
A vaccine has been approved and funded by Government to protect women against cervical cancer. Around 80% of Australian girls now receive this as part of a school-based program. From 2013, this program was also extended to boys. Since the introduction of this vaccination program, there has been a dramatic and steady decrease in genital warts among young women, and it is thought there will be similar reductions in cases of cervical cancer in the future.
The vaccine is also available to adults, via their General Practitioner or sexual health clinic. It is most commonly only available as a private prescription, as it is not funded for this use under the Australian PBS (Pharmaceutical Benefits Scheme) yet. It is quite expensive - three doses are required over 6 months, at a
cost of approximately $150 per dose (that is, a total of $450). Some
people may be able to claim some of the cost of the vaccine if they have
private health insurance, depending on their policy
However, several states are offering catch up and other programs for free vaccinations for men who have sex with men:
In NSW: Until 31st December 2018, a free vaccination for HPV is available to guys aged 20-34 through public sexual health clinics.
In Victoria: A free catch-up HPV vaccination program is offered until 31 December 2018 for men who have sex with men up to 26 years of age who may have missed the school aged vaccination program.
In South Australia: A
free HPV vaccination program is offered until 31 July 2019 for men who
have sex with men up to 26 years of age. For more information, see the SAMESH website.
In Western Australia: A free catch-up HPV vaccination program
is provided to men who have sex with men at M Clinic. Royal Perth
Hospital Sexual Health Clinic also provides free vaccination to men who
have sex with men.
Vaccines have been developed to protect against HPV, including the strains which are most likely to cause anal cancer.
Some studies have shown that men who have already been exposed to HPV could still benefit from anti-HPV vaccines. Even if you already have been exposed to one or more of the HPV strains against which the vaccine is targeted, you may still potentially benefit from the vaccine by protection against other strains which you have not yet been exposed to. In people with evidence of prior infection, vaccination can possibly help protect from reacquisition or recurrence of infections leading to warts and other cell changes, including cancer. However, further study is needed in this area.
Talk to your doctor about vaccination for HPV.
See also Can Anal Cancer be Prevented?
Back to top
Genital & Anal Warts
What are Genital & ANAL Warts?
Genital warts are one or more growths on the penis, vagina, scrotum or groin. Anal warts are virtually identical growths occurring on the anus. They can be raised, flat or cauliflower-shaped. They usually do not hurt, although are occasionally itchy.
They typically appear within weeks or months after sexual contact with someone. However, most people with HPV have no symptoms, are unaware of their infection, and so will not realise they can pass them on.
The high-risk varieties (including HPV 16 and HPV 18) are not the cause of genital warts. Genital warts themselves probably have no role in the development of HPV-related cancers. However, warts can occur at the same time as pre-cancerous conditions and it can be sometimes difficult to tell them apart.
Removal of genital & ANAL warts
Genital warts can be treated with creams, freezing, or surgery. Self-applied creams and paints, available on prescription only, can be effective at removing up to 75% of warts. The current recommended ones in Australia are Imiqimod (Aldara) and Podophyllotoxin (Condyline, Wartec).
Genital warts themselves probably have no role in the development of HPV-related cancers. However, they can occur at the same time as precancer.
Your GP may be able to remove genital warts if they have access to liquid nitrogen.
Surgery is generally used only for extensive or persistent cases.
No one treatment is better than the other. Even if removed, the warts may return several months later. Several treatments may be required.
Some genital warts disappear by themselves, but most require treatment. Removing them will not necessarily reduce the risk of passing HPV onto a partner. If warts bleed, this may increase chances of transmission of HIV during anal sex.
Cigarette smokers are more likely to develop genital and anal warts, and they generally respond less well to treatments.
There are a number of over the counter preparations that are marketed for the treatment of warts on the hands and feet. It is recommended that you do NOT use these on the genital areas – they can result in serious burning of the delicate skin.
Back to top
Anal Cancer
What is Anal Cancer?
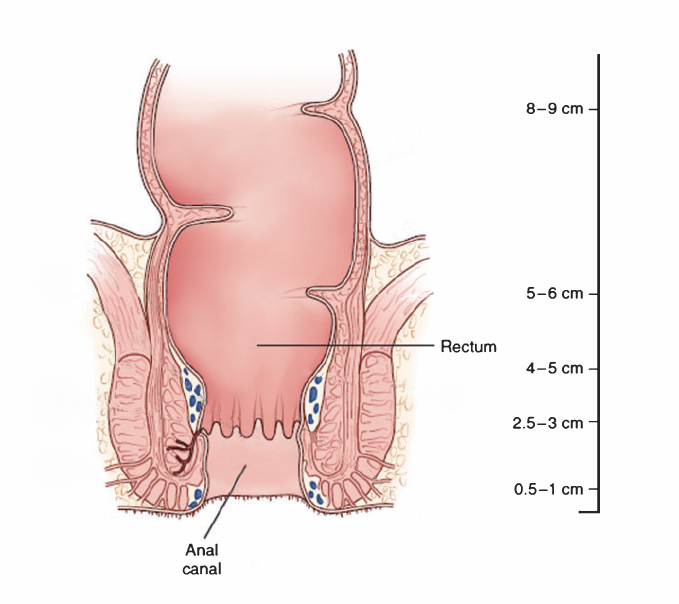
The anus extends from the anal opening to about 4 cm inside the body, where it joins the rectum. The part of the anus inside the body is called the anal canal.
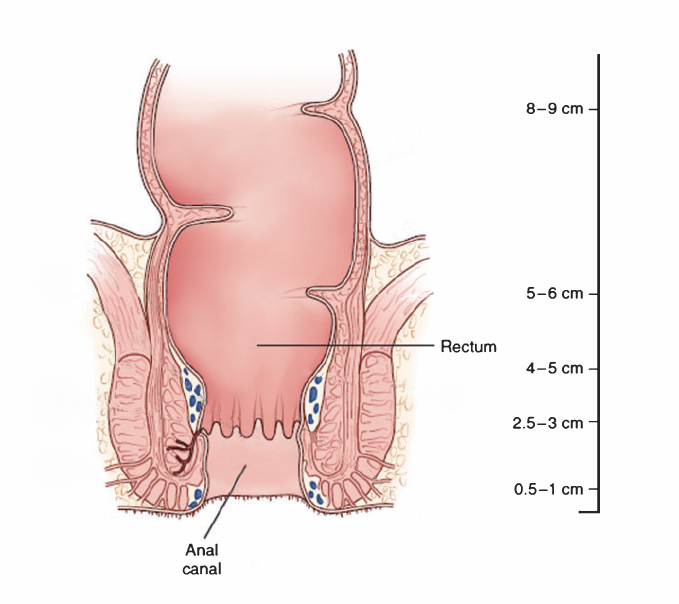
The anal canal (1)
Anal cancer occurs mainly in two places: in the junction, where the anal canal meets the rectum and in the peri-anal skin just outside the anal opening.
Anal cancer develops slowly over a period of years. It starts as a pre-cancerous condition called “high grade squamous intraepithelial neoplasia (HSIL)”, “pre-anal cancer” or “anal dysplasia”.
See also Understanding Anal Cancer Screening Results.
Anal cancer occurs when pre-cancerous changes spread to surrounding tissues and lymph glands. Spread of anal cancer is mainly through the lymph glands, although rarely it can occur through the blood.
Who Gets Anal Cancer?
Rates of anal cancer have been increasing. There are some groups of people who are at increased risk on anal cancer. These are gay men and other men who have sex with men, people living with HIV (regardless of their sexual orientation), smokers, women with a history of other genital HPV-related disease, and those receiving therapies that suppress the immune system, such as renal transplant patients. Rates are highest amongst gay men and other men who have sex with men, especially those who are HIV-positive. Rates increase with age, and more than 95% of anal cancers occur in people over 35 years of age.
PRE-ANAL CANCER
Pre-anal cancer, or HSIL, is a pre-cancerous condition but is not cancer itself. It refers to abnormal high-grade cell changes in the lining of the anal canal. Abnormal cells clustered together form a “lesion”. Most lesions don’t change and some actually shrink or disappear. There is limited consensus on the rates of progression from these high-grade cell changes to anal cancer, but calculated rates of progression are around 1 in 400 per year in HIV-positive men who have sex with men (MSM), and around 1 in 4000 per year in HIV-negative MSM. Smoking, older age, lower CD4 count and drugs that suppress the immune system probably accelerate this process.
Many people have a diagnosis of pre-anal cancer and never develop anal cancer.
See also Understanding Anal Cancer Screening Results.
MANY PEOPLE HAVE A DIAGNOSIS OF PRE-ANAL CANCER AND NEVER DEVELOP ANAL CANCER.
Symptoms of Anal Cancer
Unfortunately there are no specific symptoms of anal cancer until it is quite advanced. In advanced anal cancer there may be anal pain, bleeding, changes to the stool and noticing a lump.
However, these symptoms are also signs of many other conditions.
The presence of pre-anal cancer may be a sign that you are at a greater risk of developing anal cancer. Monitoring this should be carried out regularly by your clinician to see if there are any cancerous changes. (See Screening for Anal Cancer.)
Types of Anal Cancer
The most common anal cancer is a squamous cell carcinoma (SCC). This is linked to HPV, particularly to HPV-16.
The other anal cancer is called an adenocarcinoma, but these are no more common in gay men, compared to the general population. It is quite rare, is not thought to be related to HPV infection and may actually be a mis-classification of colon cancers.
Rates of anal cancer in Australia
Researchers from the Kirby Institute in Sydney examined the incidence of anal cancer and survival rates between 1982 and 2005. They found that, over the study period, the prevalence of these increased by 50% from 0.65 per 100 000 to 1.0 per 100 000. The annual rate of increase was two times higher in men than women.
Survival rates from anal SCCs have increased in the last twenty years. However, the most important thing to know is that early detection greatly increases the survival rate. The earlier a person is diagnosed, the better the outcome. This is why regular screening is important. (See Screening for Anal Cancer.)
Back to top
Can Anal Cancer be Prevented?
There are currently two vaccines available to protect against acquiring HPV -
both are likely to protect against the two strains of HPV that cause most anal cancers. The vaccines are most effective if given prior to
exposure to HPV, however, some research has shown that even if you have
had prior HPV exposure you may still benefit from vaccination. Further
study is needed in this area. (See Can HPV be prevented?)
There are a number of things you can do to help prevent anal cancer, including:
- Talk to your doctor about vaccination for HPV
- Talk to your doctor about having digital anal-rectal examinations (DARE) – see Screening for Anal Cancer
- Stop smoking
- Get checked by your doctor if you have any anal symptoms (e.g. anal pain, bleeding, changes to the stool, lump)
Immune-compromised people are more likely to develop anal cancer. For
HIV-positive people, it is likely that maintaining a good CD4 count will provide a
degree of protection against developing anal cancer. Some studies show that lower CD4 counts are associated with higher rates of anal cancer. Research also suggests it is important that you start HIV treatment reasonably early. Talk to your doctor about including this information in your treatment decisions, or talk to your doctor if you are concerned.
Cervical cancer in women has many similarities to anal cancer. There
have been dramatic reductions in the cases of cervical cancer in
Australia following the introduction of cervical screening (“Pap smear”)
programs.
In a similar manner, it has been proposed that early diagnosis of
high-grade anal cell changes may help prevent anal cancer. Screening is being
evaluated with anal Pap smears, by examination with high resolution
anoscopy and biopsies, and a number of new tests on anal swabs (called "biomarkers"). See Screening for Anal Cancer.
Surgical or laser removal of high-grade anal cell changes is sometimes recommended.
Unfortunately these cell changes frequently recur with currently available
treatments, particularly in HIV-positive people.
If anal cancer is found, treatment with chemoradiation can be very successful. (See Information for Men Diagnosed with Anal Cancer.)
Back to top
Anal Cancer and Gay Men
Why are gay men at greater risk?
Anal sex is a major risk factor for the acquisition of HPV and for the development of anal cancer.
A recent international study found that gay men are more likely than heterosexual men to remain infected with cancer-producing strains of HPV – particularly HPV 16 and HPV 18 –over a six-month period. This may be because the anus is more prone to acquire HPV than the rest of the genital area. The number of partners may also be a factor as it can lead to more frequent infection with a greater variety of types of HPV. More work is needed to exactly determine which sexual practices are most risky, but unprotected receptive anal sex is likely to be the easiest way for it to be transmitted.
The longer the virus stays in someone’s system, the more likely it is to do damage.
A US study found that not only does HIV infection increase the risk of HPV infection but that the converse was also true: HPV increases susceptibility to HIV infection. Anal HPV lesions may make the surface tissue of the anus more vulnerable to the entry of HIV. Some of the immune cells activated by HPV are also ones that are most vulnerable to HIV infection.
Risks for HIV-positive gay men
HIV-positive men are at greater risk of having high-risk types of HPV. A recent study found that 93% of HIV-positive gay men have at least one HPV type, compared to 64% of HIV-negative gay men. 74% of HIV-positive men had at least one high-risk HPV type, compared to 37 % of HIV-negative men.
Recent research also shows that successful treatment of HIV may reduce the risk of anal cancer for men living with HIV. It showed that men who were highly adherent to their HIV treatments (that is, were taking them as prescribed) and had an undetectable viral load, were less likely to have anal infection with the strains of HPV most associated with a high risk of cancerous cell changes. A high CD4 count also reduced the risk of infection with these strains.
not only does HIV infection increase the risk of HPV infection but the converse IS ALSO true: HPV increases susceptibility to HIV infection.
Back to top
Other HPV-Related Cancers
HPV plays a role in the development of other cancers in men, such as in the penis, and throat.
Penile Cancer
Almost all penile cancers are squamous cell carcinomas. Many of these cancers are directly attributable to HPV infection.
HPV-related penile cancer has been shown to be more likely to occur in people who have HPV-16 infection although HPV-18, HPV-6 and HPV-11 may also have a role.
The prevalence of penile cancer in Australia is low. In 2005, for instance, there were only 69 cases reported. The incidence rate for Australia is 0.7 per 100 000 people.
Penile cancer cases have not been increasing in recent times. They usually occur in older men, over 60 years of age and present with a lump or ulcer that is often painful.
Circumcised men have lower rates of the cancer. It is not clear though whether circumcising someone as an adult reduces the chances of getting penile cancer.
Giving up smoking may help prevent penile cancer.
There is currently no approved screening test to find early signs of penile cancers.
IT IS IMPORTANT TO REMEMBER THAT PENILE CANCER IS A RARE FORM OF CANCER.
Penile cancer is usually treated with surgery. This includes microsurgery (under a microscope), excision, laser surgery and cryosurgery (the freezing of abnormal tissue).
It is important to remember that penile cancer is a rare form of cancer.
Cancers of the mouth and throat
The most common cancers most closely related to HPV connection are cancers of the tonsils, the base of the tongue and the throat.
In Australia in 2005, there were 395 cases of these cancers in men and 114 cases in women. Of the cancers in he mouth and throat, cancer of the tonsils has increased the most, by about 1% per year between 1982 and 2005.
While some of these cases are not attributable to HPV infection, there are suggestions that higher numbers of sexual partners and oral sex may play a role in the increase in mouth and throat cancers.
The incidence of cancer at sites mostly related to alcohol and cigarette smoking (tongue, gums, floor of the mouth, palate and other sites within the mouth) occur at older ages and are decreasing in incidence. These are less likely to be associated with HPV infection and the decline is possibly related to a reduction in cigarette consumption.
Stopping smoking will reduce the risk of developing most cancers of the mouth and throat.
Back to top
Download